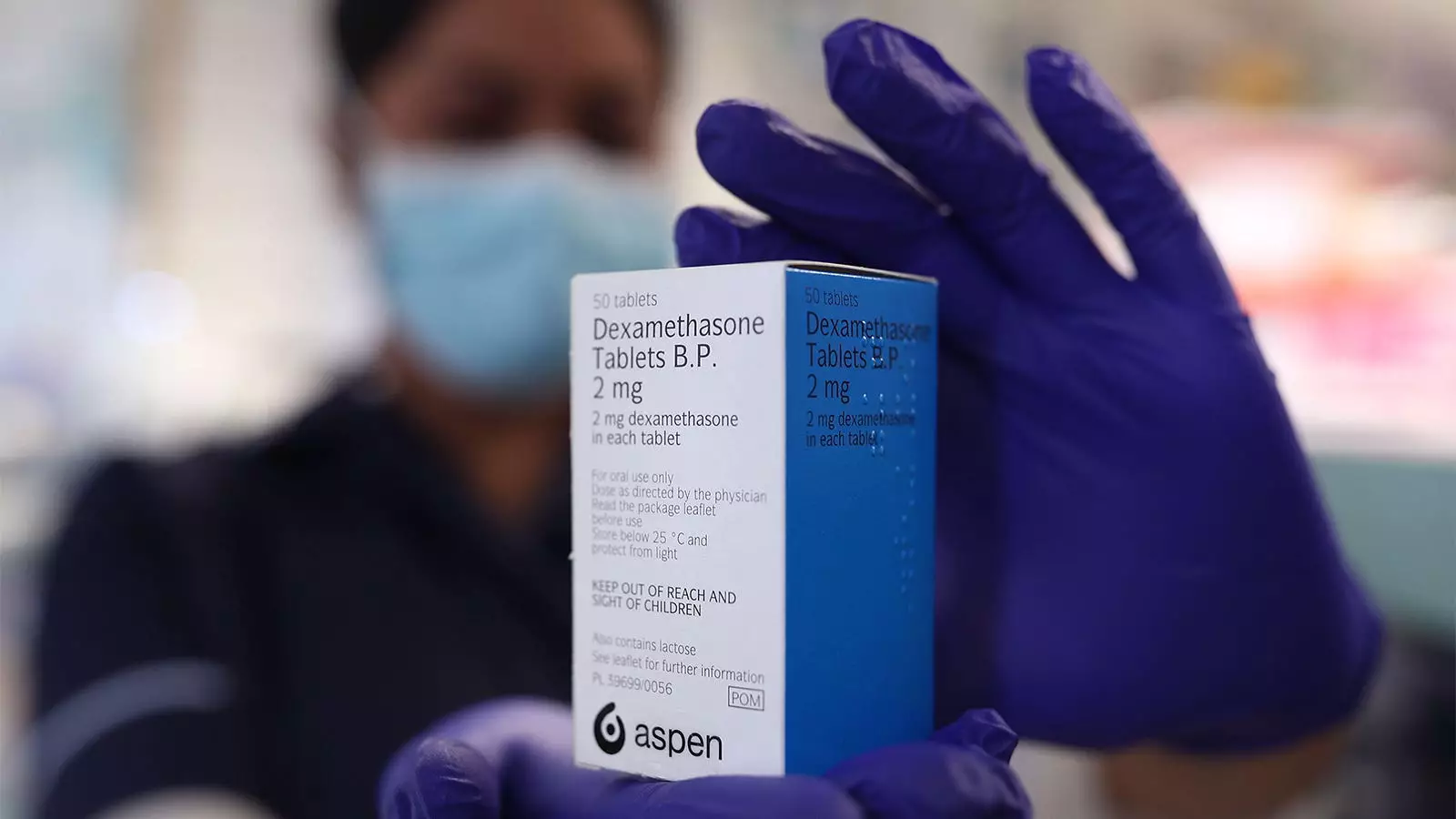
In a recent randomized controlled trial conducted in Vietnam and Indonesia, researchers found that the addition of dexamethasone to the treatment regimen for tuberculous (TB) meningitis in heavily immunosuppressed HIV-positive patients did not significantly improve survival or provide any other measurable benefits. The study, published in the New England Journal of Medicine, examined 520 HIV-positive adults receiving chemotherapy for TB meningitis and compared the outcomes of those who received dexamethasone alongside their treatment with those who received a placebo. The findings indicate that the use of dexamethasone did not yield a significant decrease in mortality rates and did not provide any measurable advantages to the patients.
Currently, most treatment guidelines recommend the use of glucocorticoids, such as dexamethasone, for all patients with TB meningitis, regardless of their HIV status. This recommendation is based on a previous trial that showed improved survival rates in Vietnamese adults with TB meningitis who received adjunctive dexamethasone. However, this trial included only 98 HIV-positive participants, and subsequent studies on steroid use specifically in HIV-positive patients with TB meningitis were lacking. Additionally, other trials involving HIV-positive patients with different types of TB have shown an increased risk of certain HIV-associated cancers with the use of glucocorticoids.
The recent trial conducted in Vietnam and Indonesia sought to determine whether dexamethasone would provide the same benefits to HIV-positive patients with TB meningitis. However, the results showed that the addition of dexamethasone did not significantly affect survival rates or offer any measured advantages. Of the participants who received dexamethasone, 44.1% died during the 12-month follow-up period, compared to 49% of those who received a placebo. The incidence of secondary endpoint events, such as immune reconstitution inflammatory syndrome, was similar in both groups. This suggests that HIV-associated tuberculous meningitis may have qualitative differences in intracerebral inflammation or mechanisms leading to death compared to TB meningitis without HIV association.
The findings of this trial have more global implications, primarily affecting adults with HIV in low-resource settings, as the majority of patients included in the study had substantial immunosuppression. It is important to note that these findings do not discount the potential benefits of dexamethasone in other patient populations or in different settings. The accompanying editorial suggests that further research is needed to determine if a smaller true effect from dexamethasone exists and was not identified in this study. Alternatively, a more targeted approach to immune modulation with therapeutics other than glucocorticoids, such as tumor necrosis factor α blockers, may be explored in specific clinical phenotypes.
While the use of glucocorticoids may not be beneficial in improving survival rates for HIV-positive patients with TB meningitis, the potential for a modestly lower risk of death still exists. Considering the severity and high mortality of TB meningitis, the use of glucocorticoids might still be justified. However, the decision to use glucocorticoids should be made in consultation with the patient’s healthcare provider and should take into account the patient’s HIV control and level of immune suppression. Additionally, efforts to expand programs like PEPFAR that improve prevention and put more people with HIV on therapy are crucial in reducing the risk of TB meningitis.
It is important to acknowledge the limitations of this study. While it included a substantial number of participants, a smaller true effect from dexamethasone may have gone undetected. Further trials with larger sample sizes are needed to determine the true impact of dexamethasone on survival rates in HIV-positive patients with TB meningitis. Another limitation of the study was that some participants received open-label glucocorticoids at some point during treatment, which may have obscured outcome differences between the groups.
The addition of dexamethasone to the treatment regimen for TB meningitis in heavily immunosuppressed HIV-positive patients did not result in a significant improvement in survival rates or provide any other measurable benefits. This study highlights the need for further research to explore alternative immune modulation therapies and targeted approaches to treating TB meningitis in this specific patient population. While the use of glucocorticoids may still be justified in certain cases, it is important for healthcare providers to consider individual patient factors and consult with multidisciplinary teams to determine the best course of treatment.

Leave a Reply