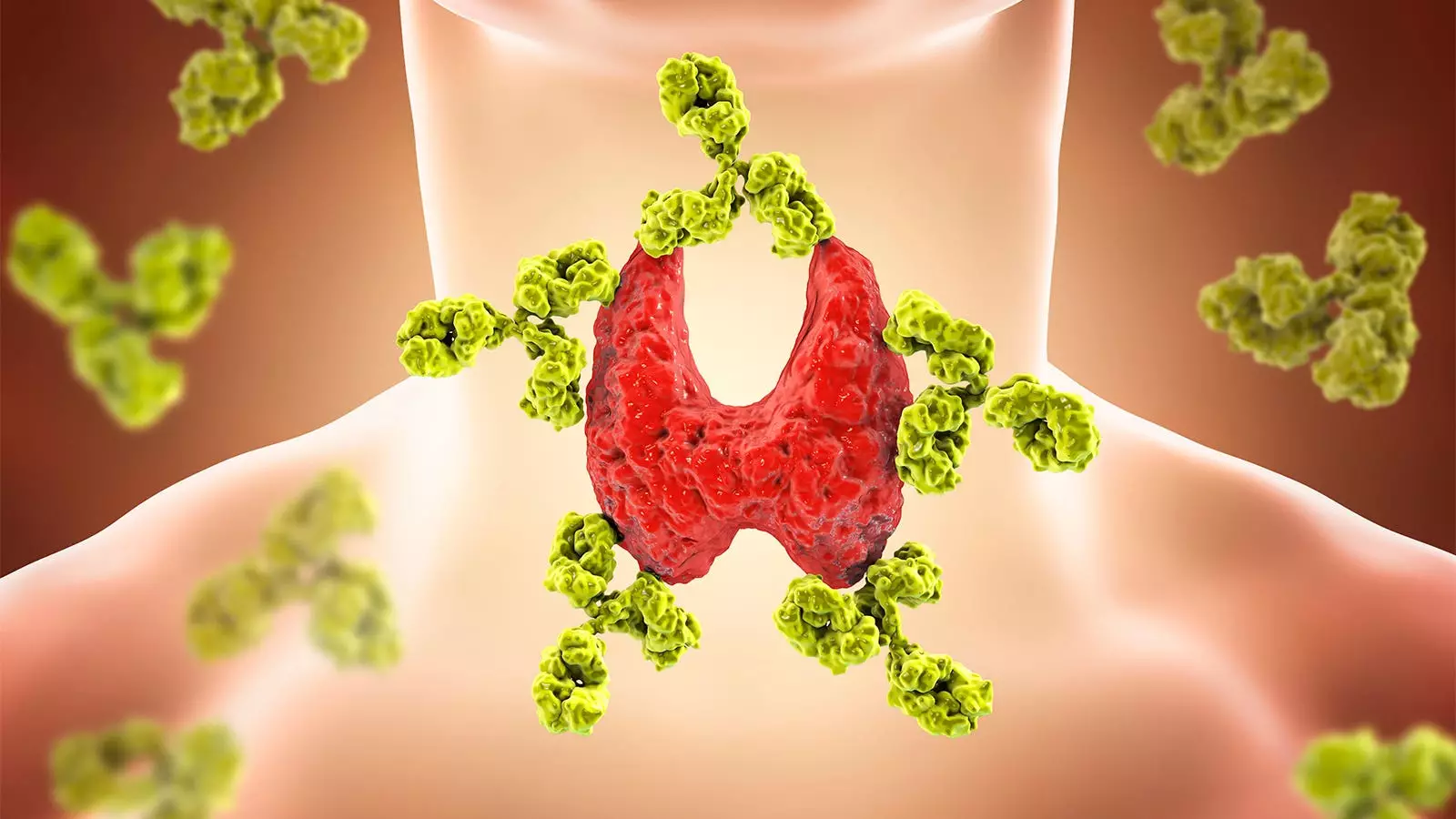
A recent extension of a randomized trial has shown that total thyroidectomy significantly improves patient-reported general health in euthyroid Hashimoto’s thyroiditis for up to 5 years. The study, conducted by Dr. Geir Hoff and colleagues at the University of Oslo in Norway, measured the quality of life using the Short Form-36 Health Survey. The initial results of the trial, published in 2019, revealed a substantial improvement in the general health score of patients who underwent total thyroidectomy compared to those who received hormonal medical management alone. In this article, we will critically analyze the findings of the study and explore the long-term effects of total thyroidectomy on quality of life.
The study included 65 patients who were followed for 60 months after total thyroidectomy. Prior to surgery, their average general health score was around 40 on a scale of 0-100. After 5 years, their score remained at around 70, indicating a sustained improvement in quality of life. These findings suggest that total thyroidectomy has long-lasting benefits for patients with euthyroid Hashimoto’s thyroiditis.
The Placebo Effect
Dr. Hoff acknowledges that the primary endpoint of the study, patient experience of “general health,” is a subjective measure that could be influenced by the placebo effect. However, he argues that the sustained improvement in quality of life after 5 years does not necessarily exclude a placebo mechanism. While placebo effects in drug trials typically diminish over time, the effects of surgery may be different. Despite the possibility of a placebo effect, the study’s results still provide valuable insights into the benefits of total thyroidectomy for patients with Hashimoto’s thyroiditis.
Potential Complications
Although total thyroidectomy led to a significant improvement in quality of life, it was not without its complications. During the follow-up period, 14% of the surgery patients experienced long-term complications, while 13 had short-term complications lasting less than a year. These complications included recurrent laryngeal nerve paralysis, hypoparathyroidism, and postoperative hematoma or infection. Dr. Hoff explains that the stringent dissection performed to achieve total thyroidectomy carried a higher risk of these complications. While the high complication rate might raise concerns, it did not appear to affect the patients’ general health scores.
Based on the study’s findings, Dr. Hoff recommends caution in considering total thyroidectomy for euthyroid patients with Hashimoto’s disease and persistent symptoms. The high complication rate, combined with the lack of a satisfactory pathophysiological mechanism to explain the results, suggests that total thyroidectomy should only be performed in dedicated centers as part of further research. It is essential to weigh the potential benefits against the risks and carefully consider each patient’s individual circumstances before choosing total thyroidectomy as a treatment option.
The extension of the randomized trial on total thyroidectomy in euthyroid Hashimoto’s thyroiditis demonstrates the long-term benefits of this surgical intervention on patient-reported general health. While the study’s findings highlight the sustained improvement in quality of life after 5 years, they also underline the potential complications associated with total thyroidectomy. Clinicians should carefully evaluate the risks and benefits and consider centralized centers for this treatment approach. Future research is needed to further explore the pathophysiological mechanisms underlying these outcomes and identify optimal strategies for managing euthyroid Hashimoto’s thyroiditis.

Leave a Reply