Herpes Simplex Virus Type 1 (HSV-1) is widely recognized for its role in causing cold sores, but recent research is uncovering its deeper implications for brain health. Traditionally viewed as a peripheral virus, HSV-1 is increasingly recognized for its potential invasiveness into the central nervous system (CNS). An insightful study conducted by researchers from the University of Colorado and the University of Bourgogne has illuminated how HSV-1 infiltrates the brain and identifies specific regions that may be vulnerable to its effects. The virus can enter the CNS notably through the trigeminal and olfactory nerves, two crucial pathways. However, the mechanisms of how this initial infection propagates throughout the brain have remained elusive—until now.
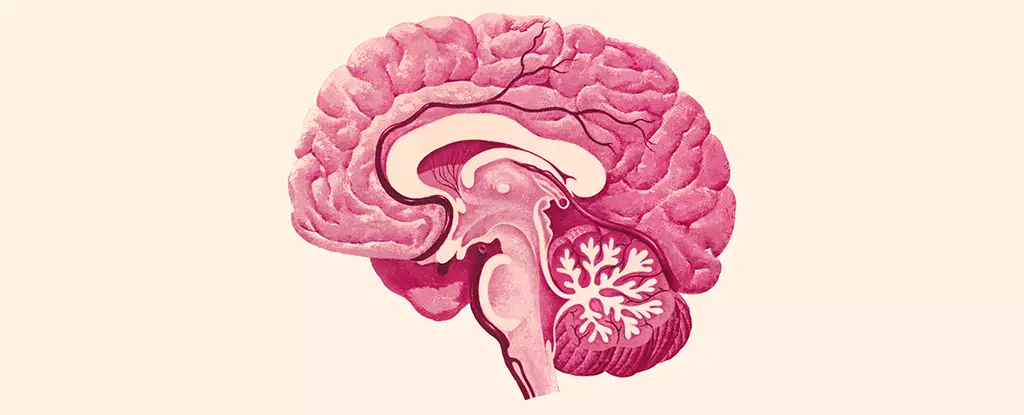
In their examination, the researchers mapped damage across various brain regions, focusing on critical areas such as the brain stem and hypothalamus. The brain stem is essential for autonomic functions including heart rate and respiration, while the hypothalamus plays a role in regulating emotions, appetite, and hormonal balance. The findings revealed that while HSV-1 did significantly affect these vital functions, some regions known for their association with memory and cognitive function, particularly the hippocampus and cortex, displayed no corresponding HSV-1 antigen presence. This distinction is particularly noteworthy, as these areas are often implicated in diseases like Alzheimer’s, highlighting potential differences in susceptibility to viral influences.
A critical aspect of understanding HSV-1’s impact on the CNS lies in evaluating the brain’s immune response. Microglia, the CNS’s resident immune cells, play a pivotal role in responding to infections and maintaining homeostasis. The study documented increased inflammation in microglia following HSV-1 interaction. Alarmingly, this immune response persisted even after the virus was no longer detected, suggesting chronic inflammation may arise from such viral encounters. Chronic activation of microglia is concerning, as it is a well-documented contributor to neuronal damage and has been linked to several neurological conditions, including Alzheimer’s disease.
As research into the intersection of HSV-1 and neurodegenerative diseases progresses, the connection to conditions like Alzheimer’s becomes more apparent. Neurologist Christy Niemeyer emphasizes that identifying the routes through which HSV-1 invades the brain and the regions it affects is crucial to understanding its potential role in fostering disease. The overlap in brain areas affected by both HSV-1 and Alzheimer’s reveals a troubling relationship potentially governed by persistent inflammation triggered by the virus, exacerbating neurodegenerative processes.
Studies suggest that the ongoing inflammation driven by persistently activated microglia may contribute to cognitive decline observed in certain Alzheimer’s patients. The chronic inflammation observed in patients with HSV-1 infections could act as a catalyst, accelerating the progression of neurodegenerative diseases. This hypothetical relationship proposes that rather than being a mere bystander, HSV-1 may initiate or exacerbate underlying mechanisms that lead to degenerative changes in brain function.
This novel study represents a significant advancement in our understanding of how HSV-1 can influence brain health and potentially contribute to neurodegeneration. However, many questions remain unanswered. Future research needs to elaborate on the precise pathways of HSV-1’s spread within the brain and its long-term consequences on cognitive function. Understanding these interactions is vital for developing targeted interventions that may mitigate the effects of the virus and possibly slow the progression of associated neurodegenerative diseases. In the grand scheme, the insights gained through such investigations could pave the way for strategies aimed at protecting brain health, ultimately contributing to better management and treatment of cognitive impairments. The intersection of viral infection and neurodegeneration merits rigorous scientific inquiry, for it holds the key to unraveling complex neurologic mysteries that could redefine therapeutic approaches.

Leave a Reply