Aging is a biological process that carries with it a complex and often paradoxical relationship with cancer risk. As we age, especially reaching our 60s and 70s, cancer risk generally escalates due to the accumulation of genetic mutations over the decades. Surprisingly, this trend does not continue indefinitely; after approximately 80 years of age, the incidence of cancer appears to diminish. This baffling phenomenon has intrigued researchers, leading to a ground-breaking study involving the behavior of specific lung stem cells that has important implications for both cancer treatment and prevention.
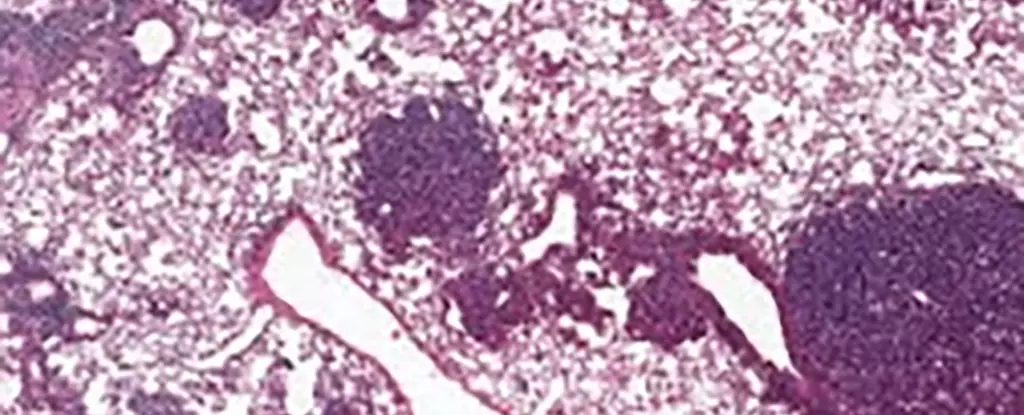
The international research team that conducted the study honed in on alveolar type 2 (AT2) stem cells in mice, which play a critical role in lung regeneration. Evidence shows that these cells are often the starting point of various lung cancers. Researchers found elevated levels of a protein named NUPR1 in older mice. This finding is significant, as it resulted in cells exhibiting characteristics of iron deficiency, despite having higher iron levels in reality. According to cancer biologist Xueqian Zhuang from Memorial Sloan Kettering Cancer Center (MSK) in New York, the aging cells behave as if they lack iron, leading to diminished renewal abilities. This phenomenon curbs not only healthy cellular regeneration but also the proliferation of cancerous cells.
The emerging conclusion is perplexing: older cells with more iron have reduced growth capacity due to an unclassic deficiency situation. This paradox may hold the key to understanding why older individuals face different cancer risks than their younger counterparts. If these mechanisms can be understood more deeply, they could shed light on strategies to potentially mitigate cancer risk or enhance treatment efficacy.
The Implications of NUPR1 on Cell Functionality
Further investigation revealed that a similar pattern occurs within human cells. Increased NUPR1 levels contributed to a reduction in accessible iron for cells, which could be manipulated to restore growth capabilities. The implications are profound—if iron metabolism can be targeted therapeutically, it may open new avenues for treatment, particularly for older patients suffering from diminished lung capacities due to conditions like long COVID.
Moreover, the research offers critical insights into ferroptosis, a specific type of cell death that is induced by iron levels. Intriguingly, older cells exhibit a decreased propensity for ferroptotic cell death due to their pseudo-iron deficiency, presenting a hurdle in the development of cancer treatments reliant on inducing this type of cell death. The study suggests that the timing of therapeutic interventions is crucial; initiating ferroptosis-based treatments earlier could vastly improve their effectiveness.
The findings also hold important lessons in cancer prevention strategies. According to Tuomas Tammela, another cancer biologist at MSK, the data implies that the events leading to cancer when we are young pose a significantly greater risk than those occurring later in life. Therefore, preventive measures, such as reducing young people’s exposure to carcinogenic agents like tobacco smoke or ultraviolet radiation, become even more critical. This paradigm shift compels society to take an active role in cancer prevention from a young age.
Future Directions and Personalized Approaches
While this research yields vital insights, it also opens up numerous questions about the intricate ways aging alters cancer biology. The necessity for personalized approaches in cancer treatments becomes increasingly clear, as factors like age, type of cancer, and other concurrent medical conditions interact and shape treatment outcomes. As Zhuang emphasizes, there remains much to explore regarding the effects of aging on stem cell function, which impacts both healthy regeneration and cancer growth alike.
Understanding the dual nature of aging in relation to cancer is not merely an academic pursuit; it directly affects clinical practices and cancer prevention strategies. Ongoing research into cellular mechanisms like NUPR1 holds promise for more effective, age-tailored cancer therapies that could revolutionize how we combat this pervasive illness throughout the human lifespan.

Leave a Reply