The diagnosis and management of autosomal dominant polycystic kidney disease (ADPKD) in patients of color poses unique challenges. Patients of Black and Hispanic descent are disproportionately affected by conditions such as hypertension and diabetes, which can potentially mask an ADPKD diagnosis. Hypertension, which is prevalent among Black individuals, can confound the diagnosis of ADPKD, as it occurs in a significant percentage of cases. This can lead to delays in screening for ADPKD, ultimately affecting the progression of the disease.
Moreover, patients with ADPKD may present with normal or only slightly reduced estimated glomerular filtration rate (eGFR), even in the presence of significant disease progression. This can make diagnosis difficult and delay the initiation of treatment. Black patients, especially those with comorbidities such as type 2 diabetes and sickle cell anemia, may experience a more rapid decline in kidney function, further complicating the diagnostic process.
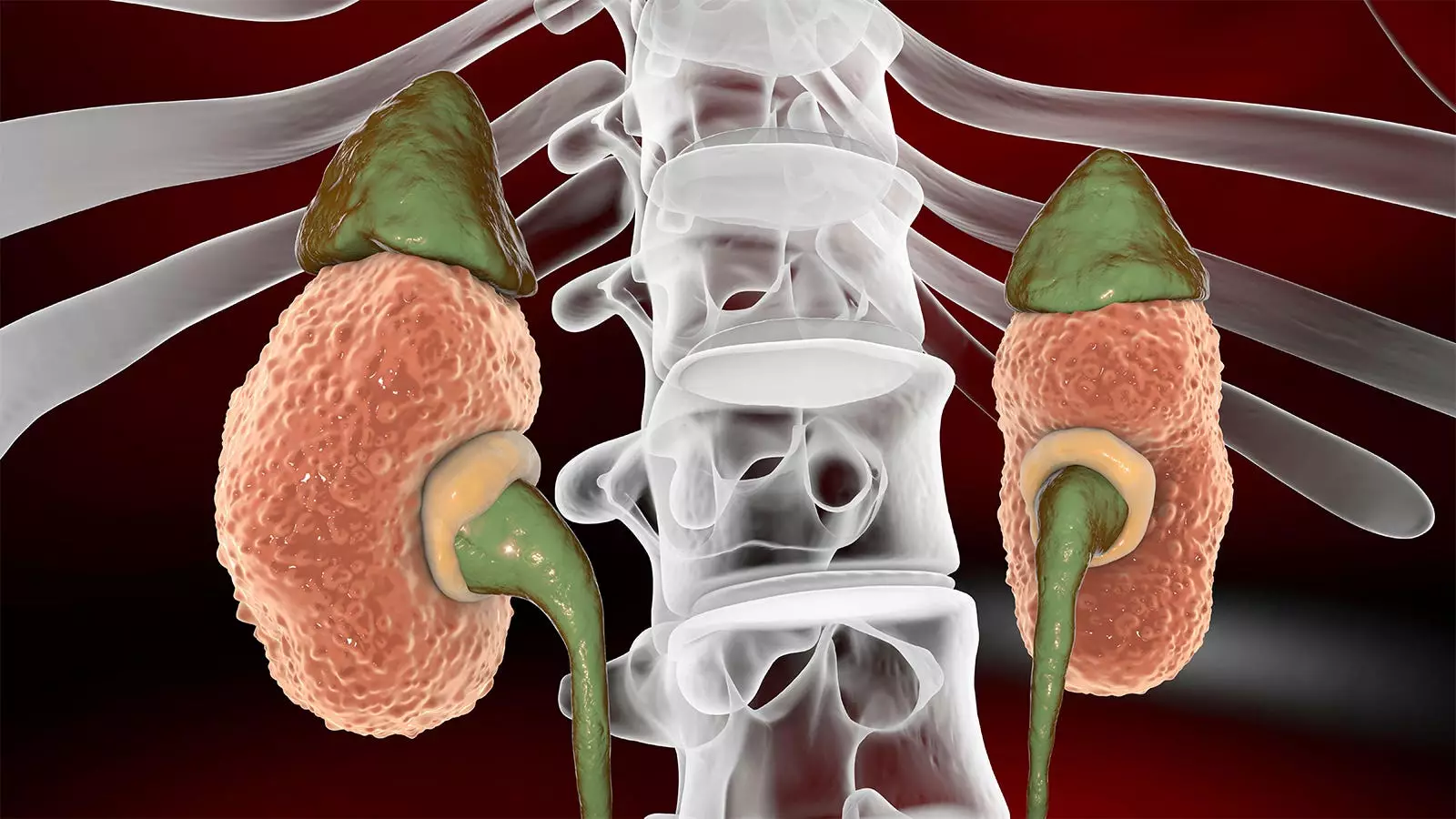
To effectively diagnose and monitor the progression of ADPKD in patients of color, healthcare providers should focus on kidney size rather than kidney function. Total kidney volume (TKV) should be measured through imaging techniques such as ultrasound, MRI, or CT scans to assess the rate of disease progression. Genetic testing can also determine if the patient carries the gene mutation, allowing for informed decision-making and risk assessment for family members.
Referring patients to a nephrologist early on is crucial for developing a comprehensive plan of action to manage ADPKD effectively. Family history of kidney failure before age 58, being overweight, and the presence of protein and albumin in the urine are additional risk factors that should be considered in the assessment and management of ADPKD in patients of color.
In addition to physical risk factors, there are structural and cultural barriers that can impact the diagnosis and management of ADPKD in patients of color. Access to medical care is a major determinant of treatment outcomes, and patients who are uninsured or living in underserved communities may face challenges in receiving timely care for ADPKD. These barriers can result in a delayed diagnosis and progression to renal failure by the time the disease is identified.
Encouraging open conversations about ADPKD within families is essential for identifying at-risk individuals and facilitating early screening and intervention. Patients should be educated about the disease and its genetic inheritance patterns, particularly if they are planning to start a family. Genetic screening can help assess the risk of inheriting ADPKD and guide family planning decisions.
Patients should be empowered to engage in discussions about their health, ask questions, and seek support from healthcare providers and other individuals living with ADPKD. Creating a supportive environment where patients feel comfortable discussing their concerns and fears is crucial for improving health outcomes. Patients of color, who may have historical reasons to distrust medical care, should be given the opportunity to voice their concerns and receive appropriate information and support.
Connecting patients with resources such as ADPKDQuestions.com can provide valuable information and support as they navigate their journey with ADPKD. Encouraging patients to seek out educational materials and support groups can help them better understand their condition and connect with others facing similar challenges. By fostering a proactive approach to patient education and support, healthcare providers can improve outcomes for patients of color living with ADPKD.

Leave a Reply