The management of acute kidney injury (AKI) in outpatient hemodialysis units presents unique challenges and opportunities. With the Advancing American Kidney Health Initiative making decreasing end-stage renal disease (ESRD) a national priority, increased attention to dialysis-requiring AKI (AKI-D) is critical. This article analyzes the current state of AKI-D management, identifies areas for improvement, and explores potential strategies to optimize patient care.
While AKI-D patients are not uncommon in outpatient hemodialysis units, the majority of patients suffer from ESRD, a condition with no potential for recovery without kidney transplantation. The treatment goals for AKI-D and ESRD patients differ significantly. AKI-D patients require close monitoring for kidney recovery and avoidance of recurrent injury, whereas ESRD patients require more aggressive fluid removal, permanent dialysis access, and transplant work-up. However, in clinical practice, it remains unclear whether management truly differs between these two patient groups.
Research on AKI-D has focused primarily on when to initiate dialysis and the optimal amount of dialysis to provide. Limited information exists about how kidney doctors monitor AKI-D patients for recovery and tailor their dialysis prescriptions accordingly. Previous studies have primarily focused on outcomes rather than process measures. A survey conducted by the American Society of Nephrology AKI Community revealed that only 35% of respondents had AKI-D protocols in their dialysis units. This knowledge gap highlights the need for a deeper understanding of AKI-D management.
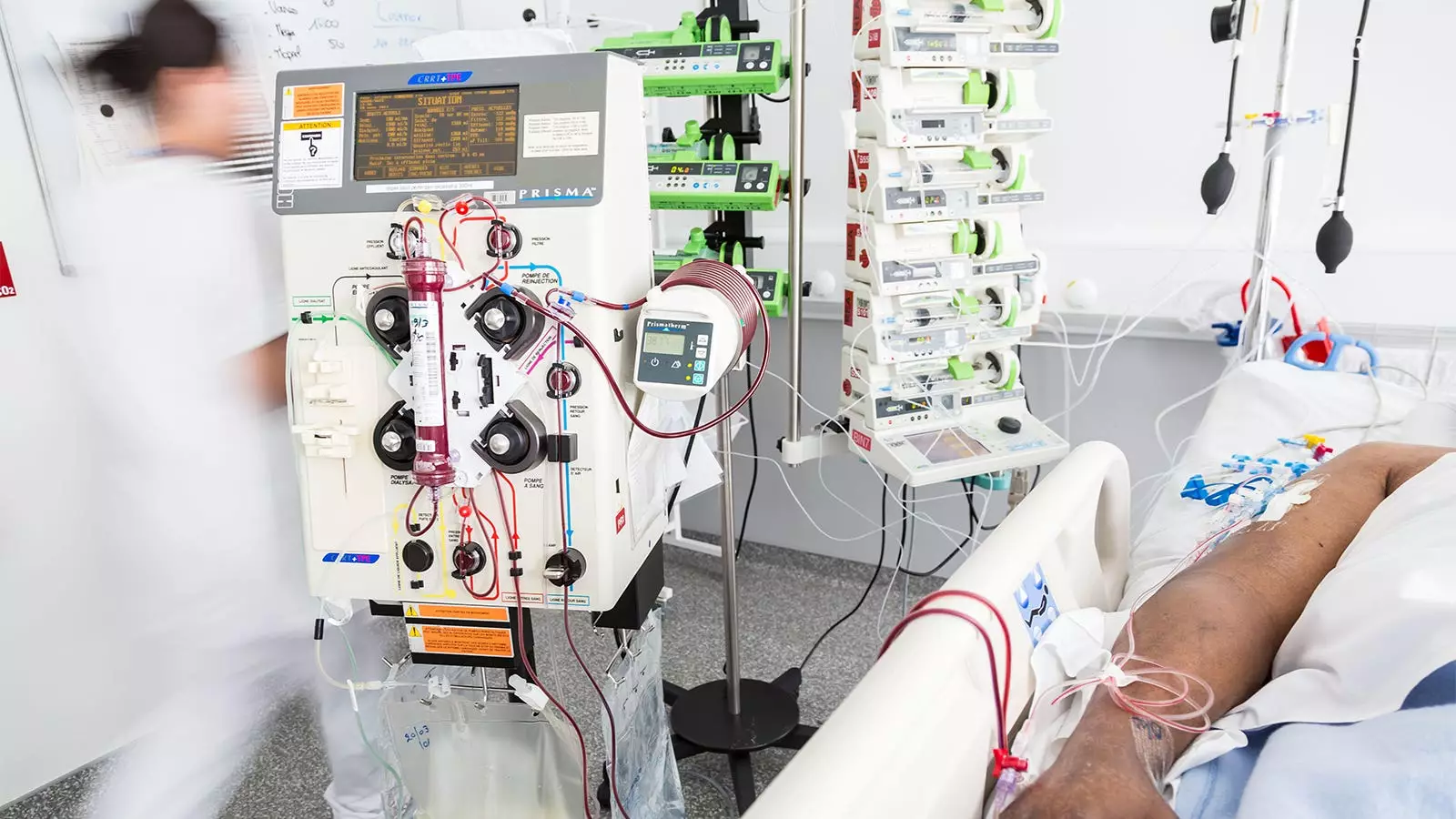
Monitoring kidney function recovery in AKI-D patients poses challenges due to ongoing dialysis treatments that artificially clean the blood, rendering blood tests ineffective in estimating kidney function. Timed urine collections have emerged as the most common method for estimating kidney function in dialysis patients. While expert groups suggest weekly urine collections, our study found that only a quarter of patients completed a timed urine collection in the first 30 days at the dialysis unit. Implementing a standardized approach to monitor recovery more frequently could lead to early detection and recognition of subtle improvements in kidney function.
When recovery is suspected, the deprescription of dialysis becomes a critical step. However, the best approach to deprescribing dialysis remains unclear. Should dialysis be stopped directly, gradually reduced in frequency, or progressively decreased in session duration? Our study revealed that most patients were abruptly stopped from three times per week to zero times per week. This finding suggests ample opportunity for implementing a more gradual approach, such as reducing dialysis from thrice-weekly to twice-weekly. Such a strategy could potentially result in cost savings and improvements in quality of life.
While there are opportunities to deprescribe dialysis among AKI-D patients, several systemic barriers hinder progress. Discontinuing or deprescribing dialysis benefits patients and leads to cost savings for the healthcare system. However, dialysis providers face financial disincentives since performing fewer dialysis sessions per week reduces their payments. Additionally, the need for extra resources to monitor AKI-D patients for recovery falls on the dialysis provider, while nephrologists receive less compensation for non-dialysis care. Overcoming these barriers will require innovative solutions and a collaborative effort among healthcare stakeholders.
Despite the challenges, optimizing AKI-D management holds great promise. Close monitoring with frequent timed urine collections can enhance the early detection of recovery. Gradual deprescription of dialysis may improve patient outcomes and reduce healthcare costs. Future research is needed to establish evidence-based protocols for recovery monitoring and dialysis deprescribing. By ensuring that no patient remains on dialysis longer than necessary, healthcare providers can offer optimal care and improve patient outcomes.
The management of AKI-D patients in outpatient hemodialysis units requires a tailored approach that differs significantly from ESRD patient care. Although challenges exist, opportunities to improve AKI-D management are evident. Strengthening recovery monitoring strategies and implementing gradual dialysis deprescription protocols can enhance patient outcomes and cost-effectiveness. By addressing systemic barriers and encouraging a multidisciplinary approach, healthcare providers can meet the goals of the Advancing American Kidney Health Initiative and improve the overall management of AKI-D.

Leave a Reply