Ovarian cancer, particularly high-grade serous ovarian carcinoma (HGSOC), presents a formidable challenge in oncology. With a grim prognosis that sees many patients succumbing within five years of diagnosis, research that elucidates potential origins and pathways of this disease is paramount. Recent investigations utilizing mouse models have pinpointed critical cellular players in the development of HGSOC, specifically within the oviducts—an area previously overshadowed in ovarian cancer research. This innovative study promises to transform our understanding of HGSOC and potentially enhance early detection and treatment strategies.
Historically, ovarian cancer diagnosis has predominantly focused on the ovaries themselves, with little attention paid to the fallopian tubes which connect the ovaries to the uterus. However, accumulating evidence suggests that many ovarian cancers could actually originate in these tubes rather than the ovaries. Research efforts spanning over a decade have revealed the genetic ties between fallopian tube lesions and ovarian tumors. Yet, while lesions have been identified, the specific cell types responsible for transitioning these precancerous states into malignancy remain elusive.
The findings from the recent studies led by pathologist Alexander Nikitin, affiliated with Cornell University, indicate a pivotal shift in understanding the cellular foundations of HGSOC. Through meticulous research into the mouse oviduct, Nikitin and his team have cataloged the various cell types present, thereby laying the groundwork for identifying the culprits behind this aggressive cancer.
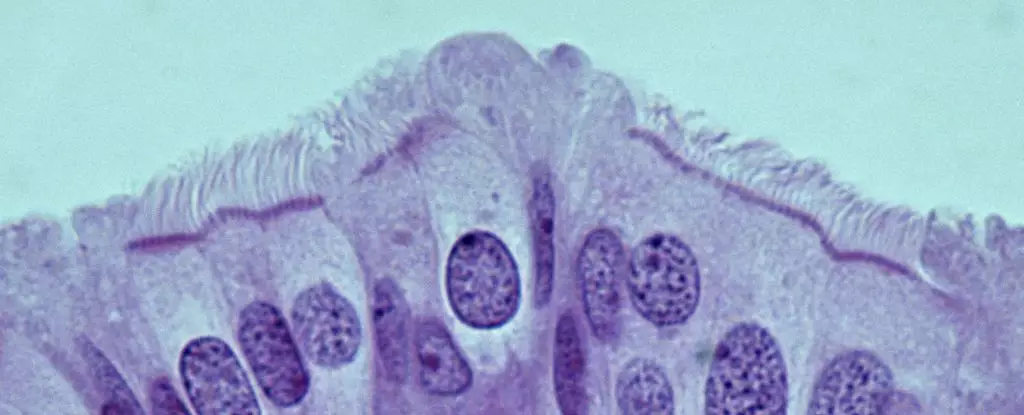
A distinguishing aspect of this study is its focus on pre-ciliated cells within the oviducts. Unlike earlier assumptions that stem cell populations were primary instigators of HGSOC, research outcomes demonstrate that pre-ciliated cells, which are in transition from stem cells to fully differentiated ciliated cells, are the more likely candidates for tumorigenesis. This nuanced understanding suggests a significant departure from previous conceptions, emphasizing the role of transitional biology in cancer development processes.
The identification of two specific genetic mutations associated with HGSOC revealed their detrimental effects on these pre-ciliated cells. Remarkably, when these mutations were present in the mouse models, they catalyzed a cascade of events leading to cancer formation. This correlation drives home the message that disturbances in cilia formation—involved in critical cellular processes—may underlie not only ovarian cancer but possibly other forms of malignancies like pancreatic cancer.
The implications of these findings extend far beyond the mouse model. If parallel mechanisms are present in human cellular biology, medical practitioners may gain new diagnostic markers to facilitate early detection of HGSOC. This is crucial since 80% of HGSOC cases are diagnosed at advanced stages when treatment options dwindle. Early identification could drastically alter outcomes, giving patients a fighting chance against a disease notorious for its stealthy progression.
Going forward, further research is essential. Understanding the underlying mechanisms of tumor formation and how they may vary with other genetic mutations could unveil innovative therapeutic strategies. The intersections between cell biology and genetics in the context of cancer underscore the complexity and vigilance required in cancer research.
The exploration of cancer-prone cells in the oviduct provides a transformative lens through which to view HGSOC. Scientists have just begun to unravel the complexities of this aggressive cancer, yet the findings mark a significant leap forward. Through meticulous investigation and innovative research strategies, the hope is that future studies will not only decode the intricacies of ovarian cancer development but pave the way for effective interventions that could change the course of this life-threatening disease. As research endeavours continue to flourish, there remains optimism that these significant strides will translate into tangible benefits for patients battling ovarian cancer.

Leave a Reply