Pediatric obesity is a multifaceted issue that affects not only the physical health of children but also their psychological and social well-being. As rates of obesity have surged among adolescents, healthcare professionals are increasingly tasked with providing effective strategies to address this health crisis. The emergence of GLP-1 receptor agonists, particularly liraglutide, represents a new frontier in treatment options. However, the landscape is nuanced, raising critical discussions around their efficacy, safety, and the context in which they can be most beneficial.
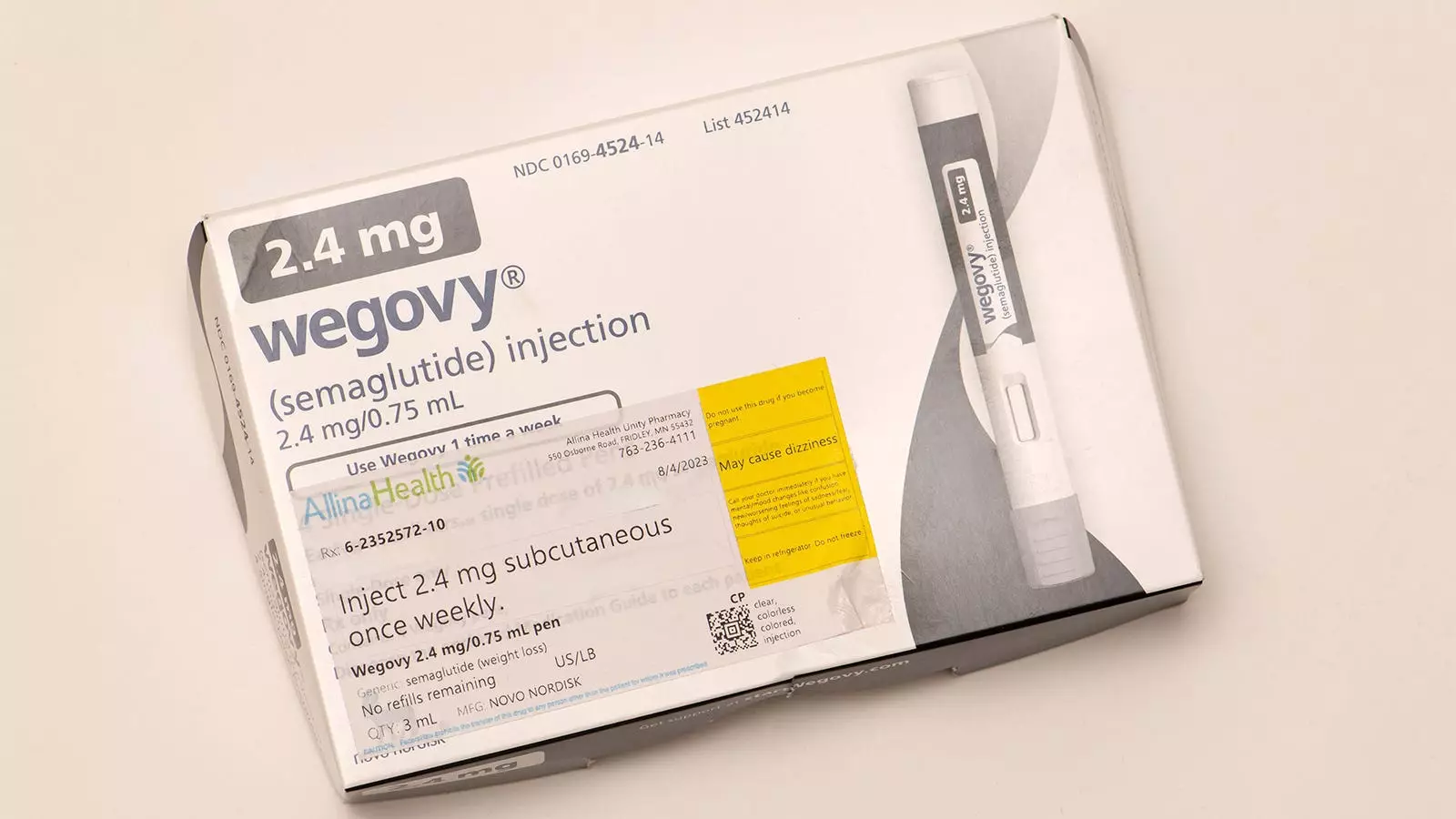
GLP-1 receptor agonists, such as semaglutide, have shown encouraging outcomes in treating obesity among adolescents when coupled with intensive lifestyle modifications. Clinical findings suggest that this combination can lead to significant improvements in not just physical health markers but also psychosocial factors. Patients report enhanced self-esteem, improved physical activity tolerance, and better sleep, illustrating a holistic approach to treatment. In the primary care setting, these medications appear to be pivotal in paving the way for healthier futures for adolescents battling obesity.
However, while such success stories are promising, the lack of FDA-approved medications for younger children under 12 poses a considerable challenge. For this demographic, despite the significant health risks associated with severe obesity, including prediabetes and psychosocial distress, practitioners have been limited to lifestyle interventions alone.
The current FDA review of liraglutide for treating severe obesity in children aged 6-12 signals a potentially transformative shift. This consideration follows a promising randomized controlled trial published in the New England Journal of Medicine. This study, involving 82 children, showed notable results; those on liraglutide experienced a decrease in BMI over a 56-week period. Yet, despite these improvements, serious questions linger around the overall well-being of children on the drug, alongside side effects and long-term impacts.
Moreover, the approval of liraglutide does not automatically equate to its adoption in treatment protocols. The practice needs to be underpinned by a comprehensive understanding of both the risks and benefits in real-world scenarios.
The potential benefits of liraglutide for younger children, while enticing, must be carefully weighed against the risks.
**Benefits** may include:
– A measurable reduction in BMI, providing a pathway to better health outcomes.
– Possible benefits regarding metabolic risk factors, though some findings remain inconclusive.
– Improvements in psychosocial aspects, as seen in older patients, although not yet clearly demonstrated for this younger age group.
On the other hand, the **risks** are significant:
– Long-term safety and effectiveness remain largely unknown, particularly concerning growth and adult height implications.
– The prevalence of gastrointestinal side effects, reported by a majority of participants, raises further concerns.
– The risk of weight regain after cessation of medication is alarming, with studies indicating that children often return to baseline weight shortly after stopping the treatment.
– Monthly injection requirements may pose compliance challenges among younger patients.
The complexity of pediatric obesity necessitates individualized treatment plans that consider both pharmacologic and non-pharmacologic strategies. While GLP-1 medications like liraglutide may provide a promising option for some children, it is essential that their use be grounded in rigorous assessments, ongoing monitoring, and clear communication with patients and families.
For healthcare providers, the proposed FDA approval of liraglutide may initially broaden the therapeutic options available but should not overshadow the need for extensive caution. The landscape of obesity treatment continues to evolve, and with advancements in medications and greater understanding of their impacts, practitioners must remain vigilant.
Ultimately, the journey of treating pediatric obesity remains fraught with challenges and opportunities. While pharmacological interventions show great promise, it is the responsibility of healthcare providers to navigate these waters judiciously, ensuring that treatments are deployed thoughtfully, with a focus on the best interests of the young patients they serve. Continued research will undoubtedly shape future treatment options, making it vital to advocate for comprehensive studies that include children in the discussion of obesity management. With careful consideration, we can hope to turn the tide against pediatric obesity, improving outcomes for an entire generation.

Leave a Reply