Pulmonary embolism (PE) is a life-threatening condition with significant morbidity and mortality rates. A recent retrospective analysis of the Pulmonary Embolism Response Team (PERT) Consortium Registry shed light on the outcomes and risk factors associated with high-risk PE. The study, conducted by researchers from the Perelman School of Medicine at the University of Pennsylvania, revealed high mortality rates among patients with high-risk PE, particularly those experiencing hemodynamic collapse. This analysis provides valuable insights into the short-term mortality and bleeding risk associated with high-risk PE and underscores the need for improved risk assessment models and care delivery methods.
The study included nearly 5,800 patients, and the results showed that in-hospital mortality occurred over five times more frequently among patients with high-risk PE compared to those with intermediate-risk PE. The mortality rate for high-risk PE patients was 20.6%, while it was only 3.7% for intermediate-risk PE patients. These findings highlight the significant impact of high-risk PE on short-term mortality and emphasize the need for prompt and effective management strategies.
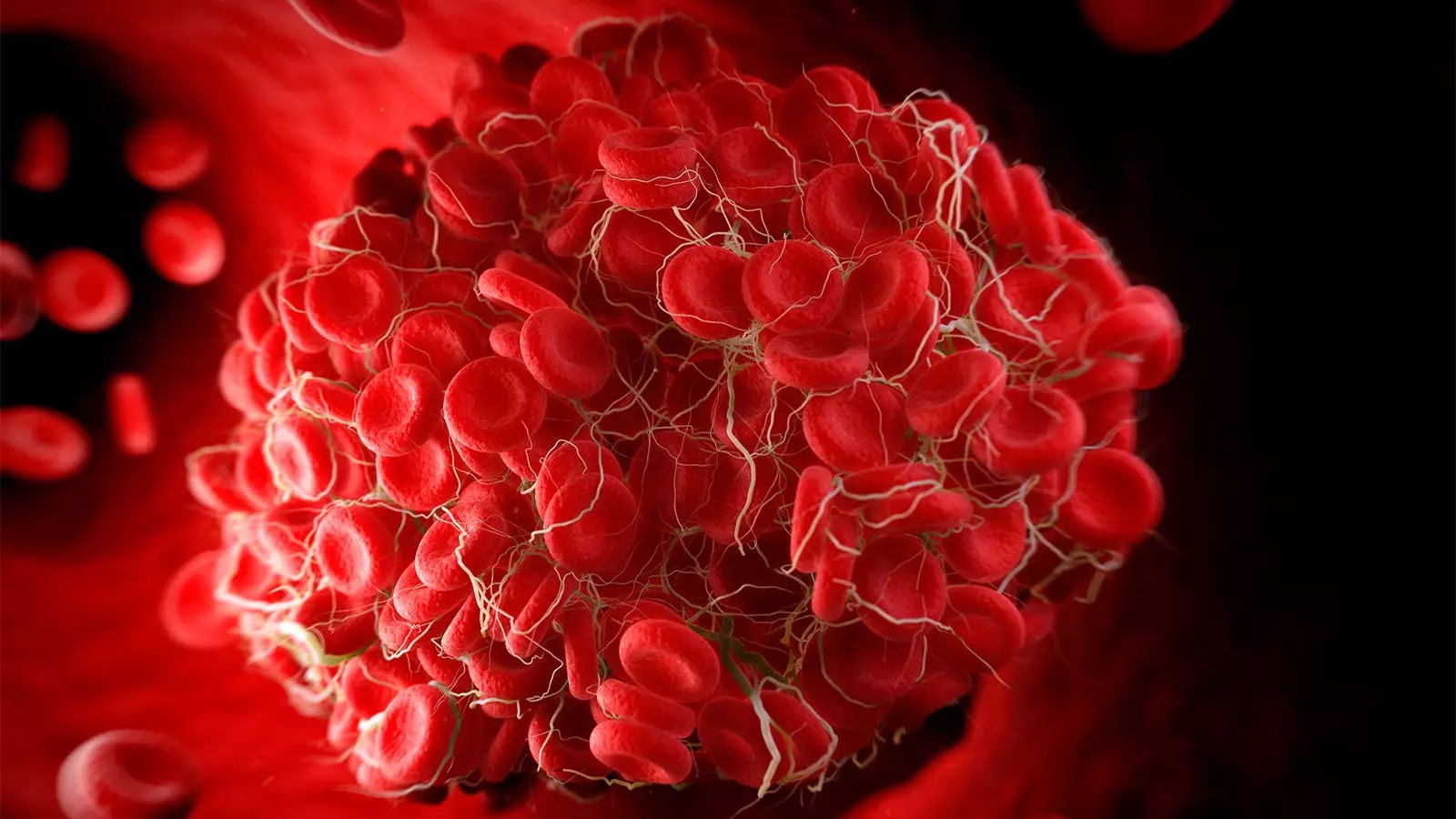
The analysis also identified several risk factors associated with in-hospital mortality in patients with high-risk PE. The use of vasopressors, extracorporeal membrane oxygenation (ECMO), the presence of an identified clot-in-transit, and malignancy were all significantly associated with increased mortality rates. These findings suggest that early recognition and management of these risk factors are crucial in improving patient outcomes and reducing mortality rates.
Patients presenting with catastrophic PE, a severe form of high-risk PE characterized by hemodynamic collapse necessitating high-dose vasopressor support, had even higher in-hospital mortality rates compared to non-catastrophic cases. The mortality rate for catastrophic PE patients was 42.1%, significantly higher than the 17.2% seen in non-catastrophic cases. Additionally, the study found that catastrophic PE patients were more likely to receive ECMO and systemic thrombolysis, highlighting the complexity and severity of this condition.
Despite advancements in PE care, the mortality rates associated with high-risk PE remain substantial. This study emphasizes the need for universally accepted definitions for high-risk PE and the development of novel metrics to improve risk assessment and identify signals of efficacy. The authors suggest considering durable changes in hemodynamics, metabolic measures of tissue perfusion, and echocardiographic and proteomic-based predictors of survival and myocardial recovery. Further research in these areas will contribute to enhanced risk stratification, tailored treatment approaches, and improved patient outcomes.
While the study provides valuable insights, there are certain limitations that should be acknowledged. The data were obtained from the PERT Consortium Registry, which might not include all patients admitted to hospitals for PE without prior consultations associated with the registry. This could introduce selection bias and limit the generalizability of the findings. Additionally, patients included in the registry may have received advanced therapies, potentially resulting in shorter lengths of stay and less time spent in the intensive care unit. These factors should be considered when interpreting the results and applying them to real-world clinical practice.
The retrospective analysis of the PERT Consortium Registry highlights the high mortality rates associated with high-risk PE and identifies key risk factors contributing to poor outcomes. It underscores the need for improved risk assessment models, refined definitions of high-risk PE, and the exploration of novel metrics to guide treatment decisions. By addressing these gaps in knowledge, healthcare providers can enhance the care and management of patients with high-risk PE, ultimately reducing mortality rates and improving overall outcomes.

Leave a Reply