Axial spondyloarthritis (axSpA) represents a significant chronic inflammatory condition primarily impacting the spine and sacroiliac joints. It falls under the broader umbrella of spondyloarthritis (SpA), which also includes peripheral spondyloarthritis affecting the limb joints. Clinically, axSpA can be categorized as either radiographic, synonymous with ankylosing spondylitis, or non-radiographic. Despite differing classifications, both forms display comparable clinical manifestations, treatment challenges, and disease burden. The primary aim of axSpA management is to alleviate pain and stiffness while mitigating disease progression to preserve functional mobility and prevent deformity.
Traditionally, nonsteroidal anti-inflammatory drugs (NSAIDs) have been first-line pharmacological agents for axSpA management. However, the response to NSAIDs varies significantly among patients, with some experiencing inadequate relief from symptoms or suffering from adverse side effects. In addition to NSAIDs, alternative treatment options have emerged from various drug classes, expanding the therapeutic landscape for axSpA. This expansion is crucial, as highlighted by updated recommendations from reputable bodies like the Assessment of SpondyloArthritis International Society and the European League Against Rheumatism (ASAS-EULAR), which emphasize a multimodal approach to treatment.
Novel Therapeutics on the Horizon
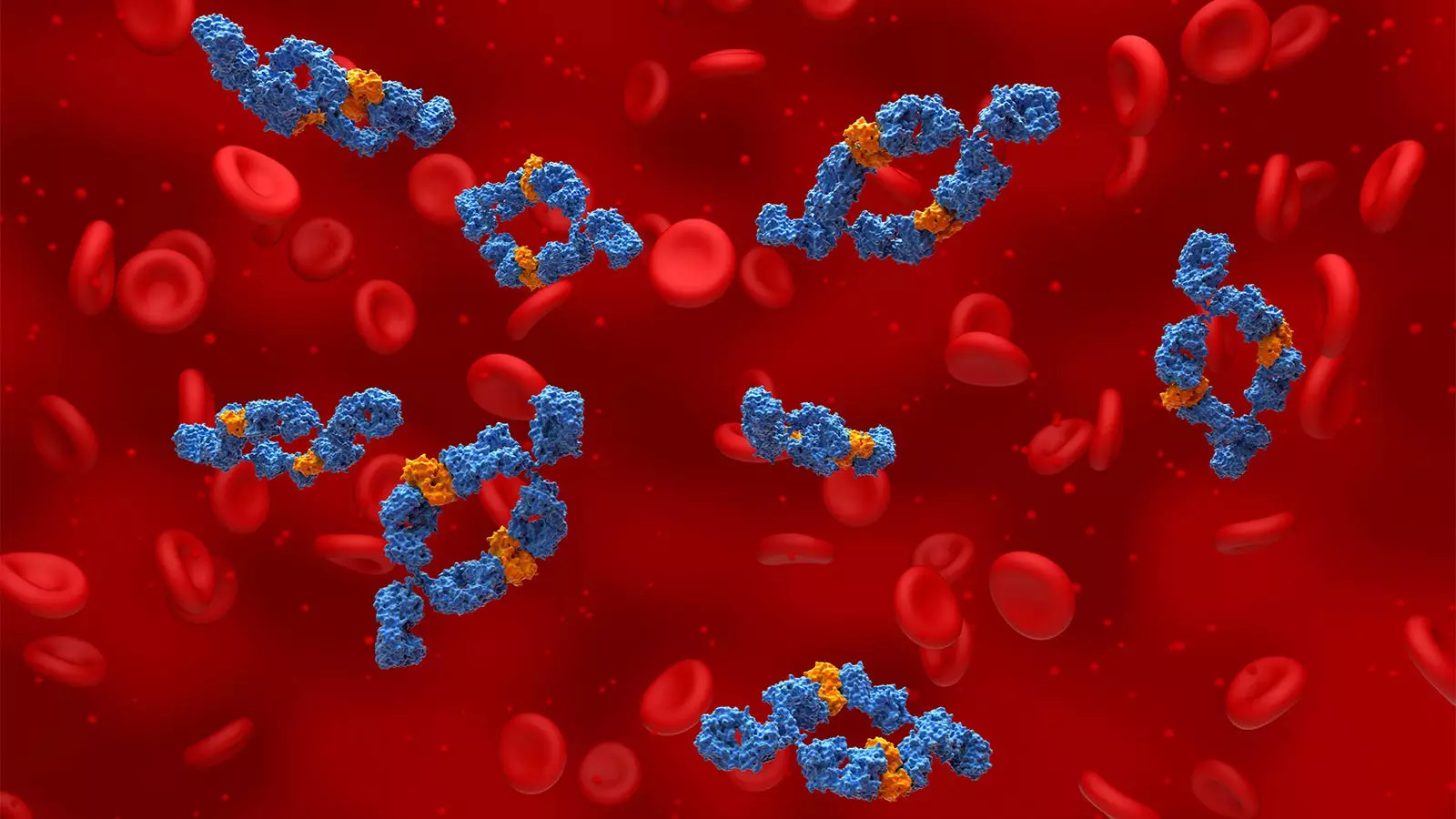
Recent advancements in the treatment of axSpA have introduced several new agents that show promise for patients who either do not benefit from NSAIDs or are unable to tolerate them. Key among these are biologic drugs, such as tumor necrosis factor (TNF) inhibitors and interleukin (IL)-17 inhibitors, as well as Janus kinase (JAK) inhibitors. A particularly notable development is the recent FDA approval of bimekizumab, an innovative IL-17A and IL-17F inhibitor, which targets specific inflammatory pathways involved in axSpA. Its approval is significant, especially for patients with active non-radiographic axSpA exhibiting objective signs of inflammation, providing a much-needed addition to existing treatment options.
Clinical trials such as BE-MOBILE 1 and BE-MOBILE 2 have brought to light bimekizumab’s potent efficacy across the axSpA spectrum, including both radiographic and non-radiographic forms. In these studies, a substantial proportion of participants demonstrated notable improvements in key assessment indices after treatment. This dual-action approach in inhibiting both IL-17A and IL-17F could potentially provide broader benefits, though head-to-head studies are needed to ascertain whether this combined action results in superior outcomes compared to single-target therapies.
The treatment choice between TNF inhibitors and IL-17 inhibitors often hinges on the presence of concomitant extra-articular manifestations, as observed by clinicians like Eric Toussirot. Although newer JAK inhibitors have also entered the arena, their use remains cautious, primarily reserved for specific patients with favorable cardiovascular profiles due to safety concerns highlighted in clinical trials. The current landscape includes several TNF inhibitors (e.g., adalimumab and infliximab) and IL-17 inhibitors (e.g., secukinumab and ixekizumab). Acknowledging these variations is supremely important for tailoring therapeutic strategies to individual patient needs.
Real-world Insights and Discontinuation Rates
Considering treatment durability and patient compliance, a recent retrospective analysis of real-world data from 2015 to 2023 revealed significant variations in treatment discontinuation rates across different therapeutic classes. JAK inhibitors exhibited higher rates of discontinuation compared to TNF and IL-17 inhibitors. Notably, many patients discontinued during the early months of treatment, primarily attributed to perceived ineffectiveness. This emphasizes the need for healthcare providers to remain vigilant in monitoring patient responses and adjusting treatment plans accordingly.
The field of axSpA management is evolving rapidly, predominantly due to the introduction of novel therapeutic agents and improved understanding of disease mechanisms. With the launch of bimekizumab and ongoing research into various treatment modalities, there is renewed hope for improved patient outcomes. As more data from clinical trials and real-world studies emerge, it remains essential for healthcare providers to remain informed and adaptable, ensuring that patients receive the most effective and comprehensive care tailored to their specific needs.

Leave a Reply