Chronic inflammatory demyelinating polyneuropathy (CIDP) is a challenging disease to diagnose and treat due to its rarity and heterogeneity. Current standard treatments like intravenous immunoglobulin (IVIG), steroids, and plasma exchange are not always effective, especially in certain CIDP phenotypes. This has prompted the search for valid biomarkers that can aid in both the diagnosis and treatment of CIDP. However, the lack of widely accepted measures for CIDP biomarkers has been a major hurdle in advancing our understanding of the disease.
In recent years, researchers have explored various biomarkers in CIDP, including autoantibodies, cytokines, complement proteins, Fc receptor modulators, and immunoglobulin G (IgG) levels. These biomarkers aim to describe nerve integrity and function, drug effects, and the activity of effector mechanisms in CIDP patients. Due to the heterogeneity of CIDP, a combination of biomarkers may be needed to identify different disease subtypes and monitor disease progression or treatment failure accurately.
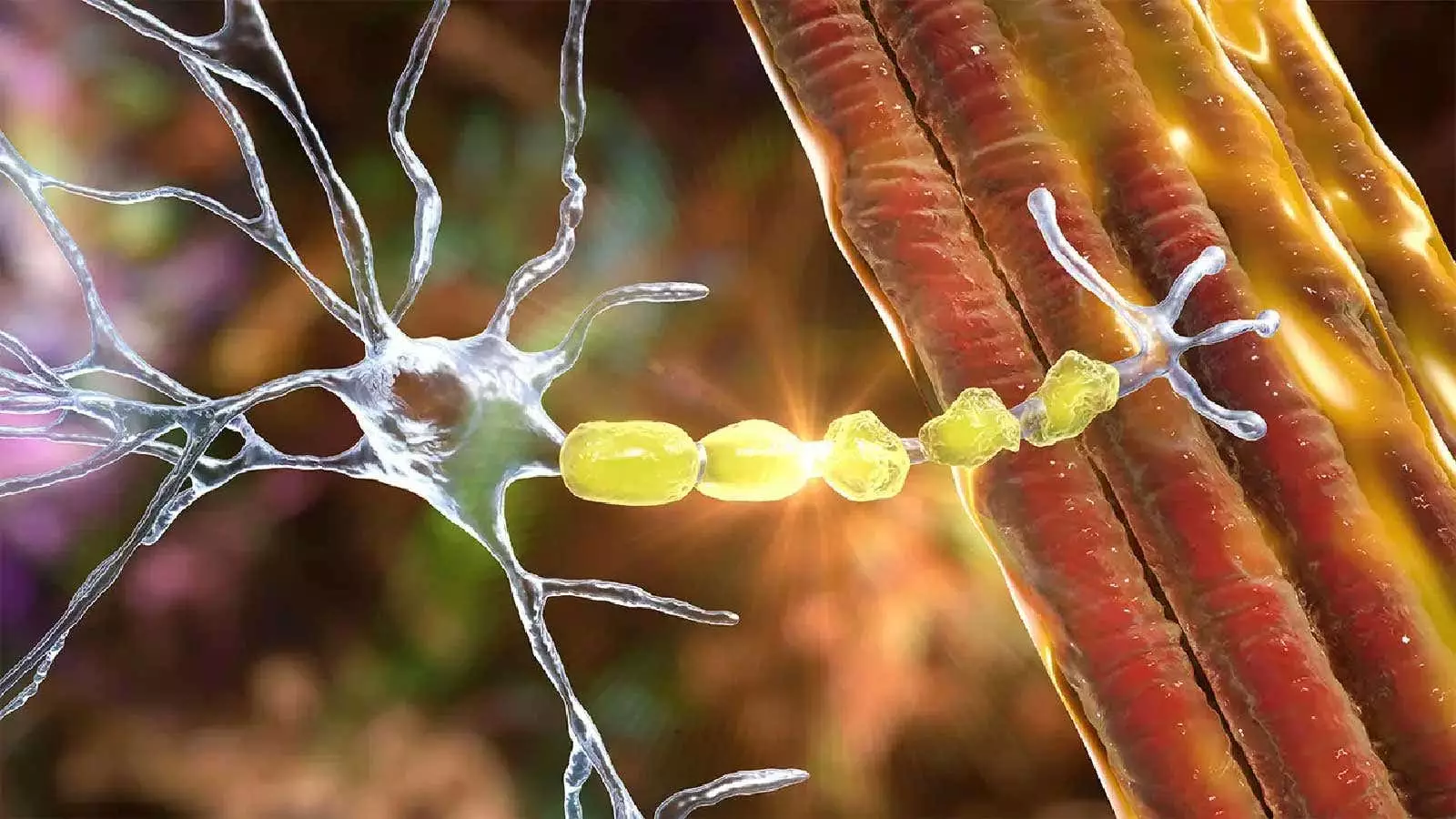
One promising biomarker is serum neurofilament light chain (NfL), which reflects axonal damage and has been linked to poor outcomes in CIDP. Studies have shown that elevated levels of serum NfL may indicate disease activity and predict progression in CIDP patients. Additionally, specific autoantibodies like anti-neurofascin-155 and anti-contactin-1 have shown potential as biomarkers for IVIG resistance in patients with autoimmune nodopathies.
One ongoing project, known as INCbase, aims to establish a registry and biobank for CIDP patients to collect biosamples for biomarker exploration. This international effort seeks to identify novel biomarkers that can improve diagnostic accuracy and disease monitoring in CIDP. By collecting data from a diverse group of patients, researchers hope to uncover new insights into the pathophysiology of CIDP and develop more effective treatment strategies.
Imaging techniques, such as magnetic resonance neurography (MRN) and ultrasound, have also emerged as valuable tools for assessing nerve damage in CIDP. MRN, in particular, offers high-resolution imaging that can visualize nerve continuity, integrity, and pathological changes with greater precision than standard MRI or electrodiagnostic tests. Studies have shown that imaging modalities like MRN and ultrasound can differentiate CIDP patients from healthy controls based on nerve morphology and signal intensity.
Despite significant advancements in biomarker and imaging research, several challenges remain in the field of CIDP diagnosis and treatment. The lack of standardized biomarkers and imaging protocols limits their widespread clinical use and hinders the development of targeted therapies for CIDP. Future studies should focus on validating existing biomarkers, exploring new imaging modalities, and integrating biomarker data into clinical practice to personalize treatment approaches for CIDP patients.
The search for reliable biomarkers and imaging techniques in CIDP is essential for improving the accuracy of diagnosis, monitoring disease progression, and predicting treatment responses. By leveraging these innovative tools, clinicians and researchers can advance our understanding of CIDP’s complex pathophysiology and enhance patient outcomes in the future.

Leave a Reply