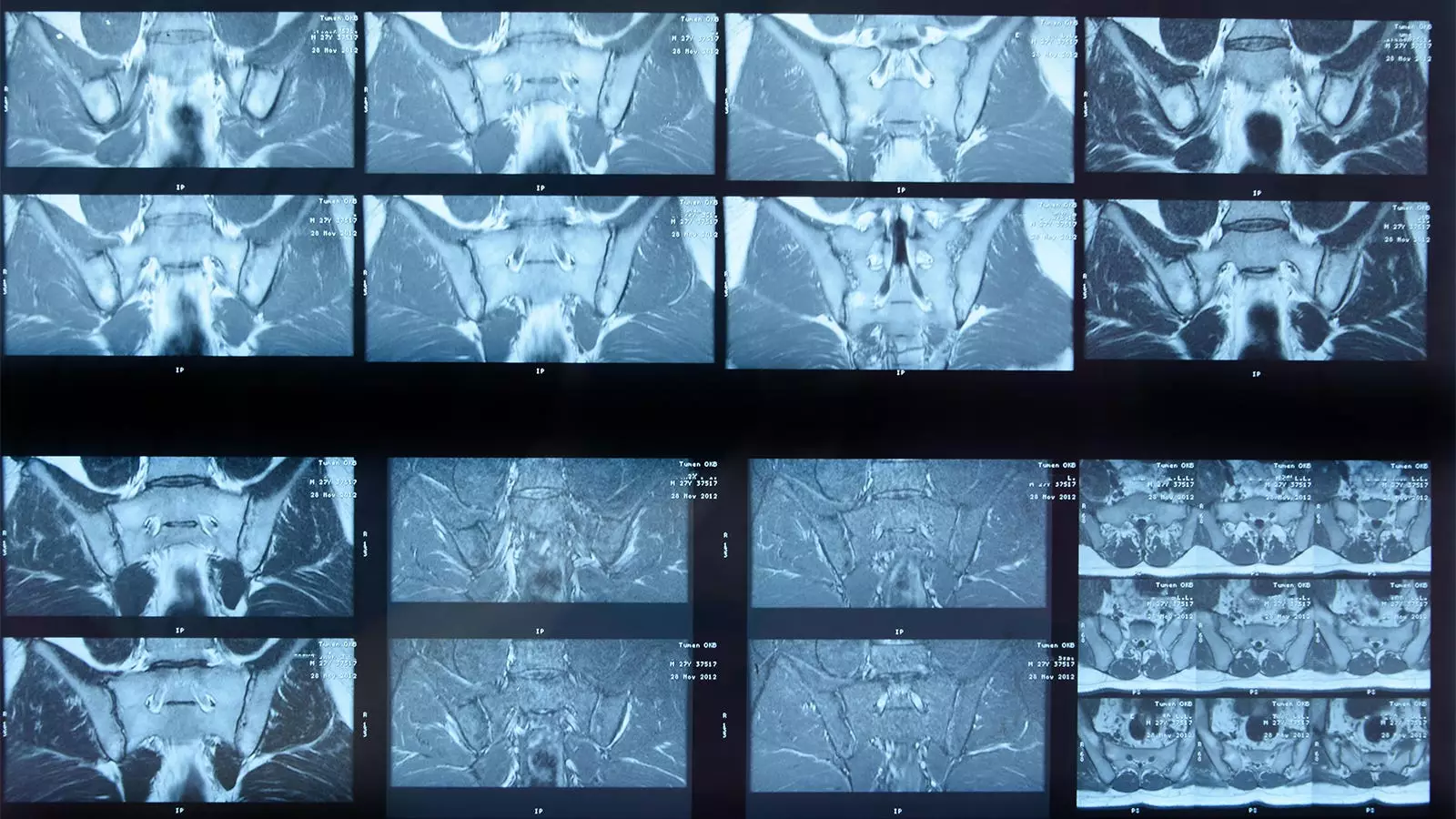
Artificial intelligence (AI) continues to revolutionize the field of medicine, particularly in diagnostic processes. Among its promising applications lies the ability to analyze medical imagery, including magnetic resonance imaging (MRI) scans. A recent study has provided clarity on the efficacy of a deep learning algorithm designed to detect inflammation in the sacroiliac joints (SIJs) of patients suffering from axial spondyloarthritis (axSpA). While the findings highlight certain strengths of the artificial intelligence algorithm, they also reveal limitations that necessitate a cautious approach to its real-world applications.
The research, conducted by a team led by Joeri Nicolaes, PhD, at UCB Pharma in Brussels, Belgium, assessed the performance of an AI algorithm against a panel of human expert readers. The panel consisted of three individuals who represented the “gold standard” for interpretation, analyzing a total of 731 MRI images. The algorithm and human readers reached concordant conclusions on 543 images: both identified inflammation in 304 instances and agreed on the absence of inflammation in 239 cases.
The study’s quantitative outcomes were revealing yet sobering. With an absolute agreement rate of 74%, sensitivity of 70%, and a specificity of 81%, the algorithm’s performance was statistically acceptable but not remarkable. The researchers noted that the algorithm’s identification was flawed in several cases—132 instances of inflammation were missed, and it erroneously flagged inflammation in 56 images deemed clear by human experts. Those discrepancies further underscored the importance of contextual clinical information often considered by human readers, which the algorithm lacked.
Understanding the Implication of Results
While the performance metrics yielded a mix of success and shortcomings, it’s essential to contextualize these findings. The authors acknowledged inherent limitations in the criteria used to define inflammation. They highlighted that conservative definitions often skew results, and expert readers could rely on additional clinical data (e.g. C-reactive protein levels and HLA-B27 positivity) that an AI system could not access.
Notably, the researchers also pointed out that the expertise of the readers in the study might outstrip that of typical rheumatologists or radiologists in real-world scenarios. This observation raises pertinent questions about the AI algorithm’s practical utility, especially in settings with less experienced clinicians. While the AI can provide consistent results, human interpretation will always require a degree of judgment that technology has yet to perfect.
The study was deeply rooted in a robust dataset taken from two UCB-funded clinical trials: RAPID-axSpA and C-OPTIMISE, comprising over 700 patients with a mean age of 34. Both trials had strict eligibility criteria, ensuring that participants were actively experiencing disease symptoms. However, an important limitation emerged, as the AI algorithm found itself unable to process images from certain patients due to technical constraints, resulting in lost opportunities to analyze a significant number of patients.
These methodological details underscore a pressing need for ongoing refinement of AI systems, ensuring that they are compatible with various MRI protocols and image qualities prevalent in clinical settings. Furthermore, the reliance on a narrow participant demographic—predominantly white and male individuals—indicates a need for broader representation in future studies to ensure the algorithm’s applicability across diverse patient populations.
Looking Ahead: Future Directions for AI in Medical Imaging
In light of the findings, there are actionable insights and future directions that can strengthen the integration of AI in clinical practice. Updating the AI algorithm to encompass evolving criteria for SIJ inflammation, as well as incorporating the capability to assess structural damage—a critical consideration in treatment planning—should be prioritized. Moreover, systems designed to collaborate with and support human decision-making appear to be more beneficial than those intended to replace clinical judgment outright.
As healthcare technologies advance, striking a balance between leveraging AI’s objectivity and preserving the nuanced understanding that expert readers bring to the table will be crucial. Ultimately, this approach may not only elevate diagnostic accuracy but also enhance patient outcomes in conditions like axial spondyloarthritis.
The advent of AI in the realm of diagnostic imaging presents both exciting opportunities and formidable challenges. While the study regarding the deep learning algorithm’s ability to detect SIJ inflammation in axSpA demonstrated acceptable performance metrics, outright reliance on its findings should be tempered with caution. As research continues to evolve, so too must our expectations of AI’s role in complementing the indispensable expertise of human clinicians. The path forward should focus on collaboration, continual improvement, and fostering a deeper understanding of the ways in which AI and human expertise can work hand in hand to enhance diagnostic accuracy in medicine.

Leave a Reply