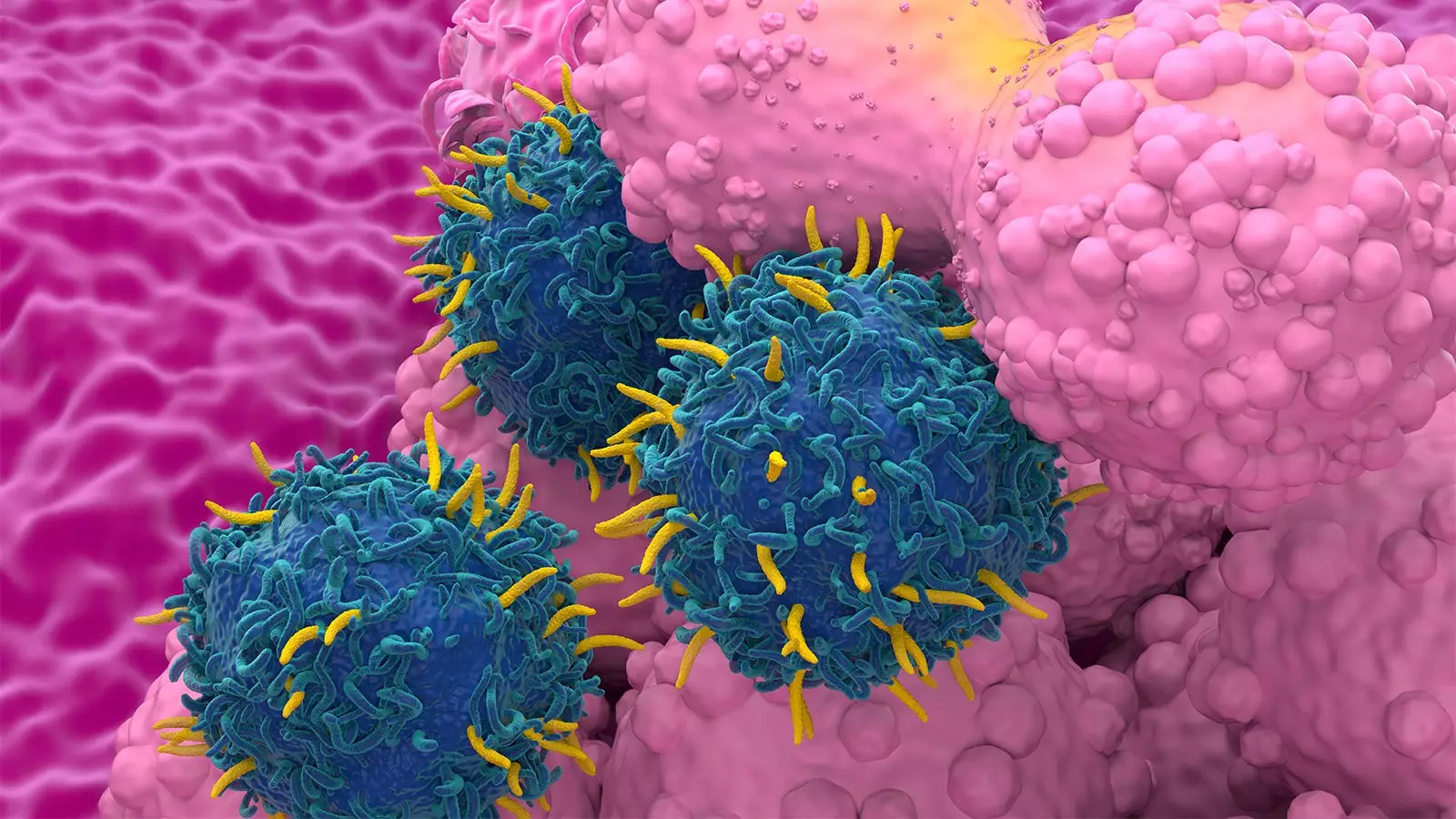
CAR T-cell therapy has gained significant attention in recent years as a promising treatment option for certain types of cancers. However, concerns have been raised regarding the potential risk of developing second primary malignancies (SPM) following this innovative therapy. A systematic literature review and meta-analysis shed light on this issue, providing valuable insights into the association between CAR T-cell therapy and SPM.
The analysis revealed a 5.8% rate of SPM among 5,517 patients who underwent CAR T-cell therapy, with a median follow-up of 21.7 months. Interestingly, the rate of SPM did not vary based on the type of disease treated or the specific CAR T-cell product used. Factors such as study setting (clinical trial vs real-world experience), longer follow-up duration, and the number of prior therapies before CAR-T treatment were associated with a higher risk of SPM. These findings challenge the assumption that CAR T-cell therapy poses a higher risk of developing SPM compared to standard-of-care treatments.
A meta-analysis that compared CAR T-cell therapy with standard-of-care treatments demonstrated nearly identical rates of SPMs (5.0% vs 4.9%). These results suggest that the risk of SPM associated with CAR T-cell therapy may not be as substantial as previously thought. Dr. Kai Rejeski of Memorial Sloan Kettering Cancer Center noted that the findings question the necessity of a black-box warning label by the FDA, which was instituted following reports of SPMs associated with CAR T-cell therapy.
The study emphasized the importance of considering various factors when assessing the risk of SPM following CAR T-cell therapy. Factors such as patient age, follow-up duration, the type of CAR T therapy received, initial diagnosis, and prior treatments all play a role in determining the likelihood of developing SPM. Notably, the analysis highlighted that factors unrelated to CAR T-cell therapy were more strongly associated with the development of SPM, underscoring the need for a comprehensive evaluation of these risk factors.
The findings of the study underscore the need for more extensive and long-term data to better understand the relationship between CAR T-cell therapy and SPM. Patients and healthcare providers must interpret these findings cautiously and communicate the potential risks associated with this therapy effectively. Dr. Rejeski emphasized the importance of educating patients about the risks while providing context and perspective based on the available evidence.
The analysis of CAR T-cell therapy and the risk of second primary malignancies provides valuable insights into a critical aspect of this innovative treatment modality. By carefully evaluating the factors influencing the development of SPM and comparing the rates with standard-of-care treatments, researchers have shed light on the safety profile of CAR T-cell therapy. Moving forward, continued research and monitoring are essential to further elucidate the long-term implications of this groundbreaking therapy.

Leave a Reply