The recent approval of Eli Lilly’s groundbreaking obesity medication, Zepbound, for patients suffering from obstructive sleep apnea (OSA) marks a significant advancement in the healthcare landscape. With the Centers for Medicare & Medicaid Services (CMS) now allowing Medicare drug plans to cover this treatment under specific conditions, we must delve into the implications of this policy change for both patients and healthcare providers.
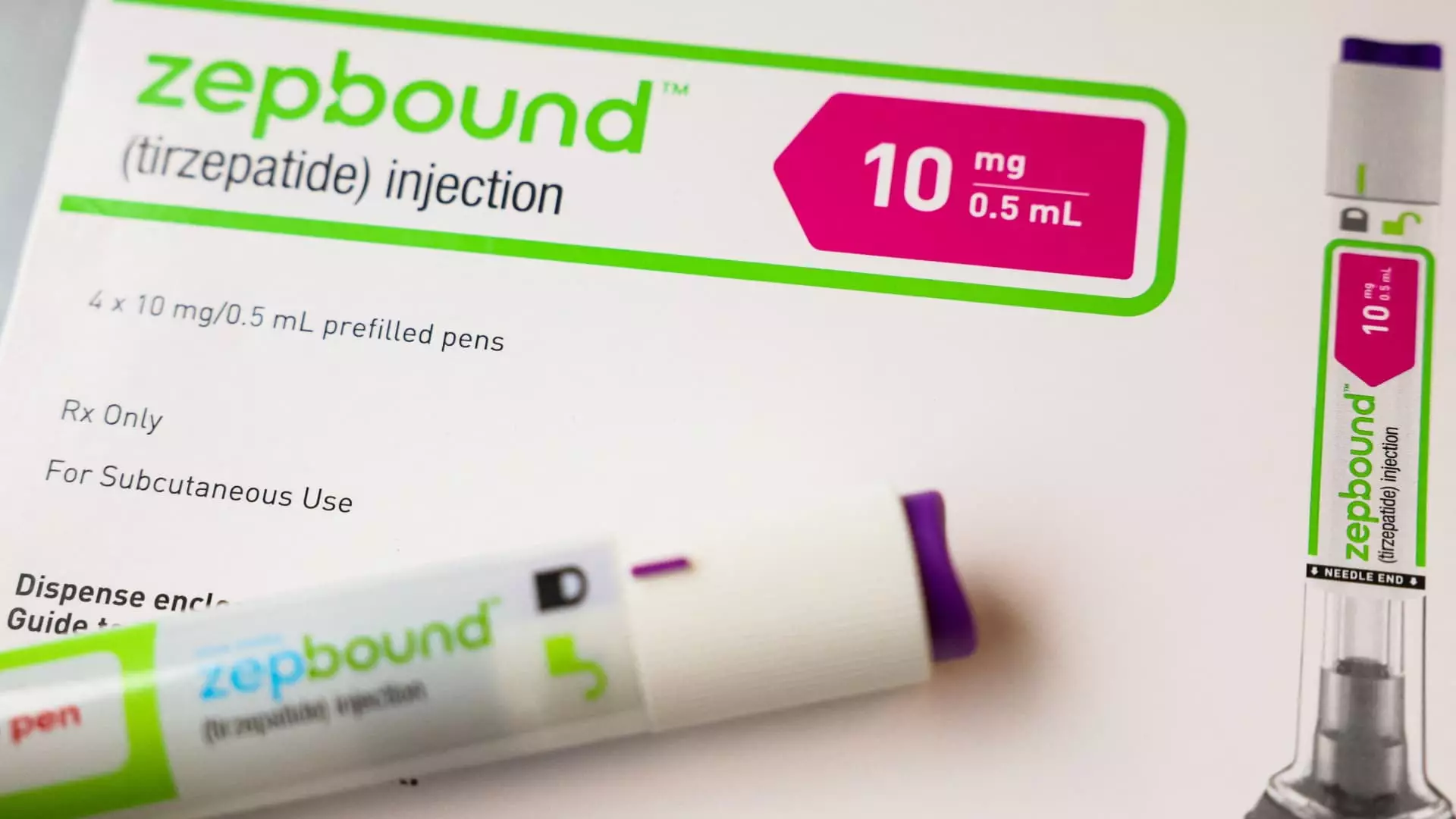
Zepbound, an injectable drug priced at approximately $1,000 per dose before insurance, has generated considerable interest over the past year. Its FDA approval on December 20 was a landmark event, as it designated Zepbound as the first pharmacological agent specifically cleared to treat moderate to severe OSA in individuals dealing with obesity. With an estimated 20 million Americans affected by OSA, this approval has the potential to touch a vast demographic of patients who have long been underrepresented in targeted treatment options.
This allows a unique intersection of obesity management and sleep disorder treatment that could help to improve the quality of life for many individuals. In particular, patients who have faced barriers in accessing treatment for their sleep-related breathing interruptions will now find Zepbound within their reach, provided they meet certain criteria set forth by Medicare.
While the inclusion of Zepbound in Medicare coverage is welcomed, the CMS has made it clear that the regulations governing prescription drug coverage remain rigid. According to a spokesperson for the agency, the approval process will require healthcare providers to demonstrate that the drug is being utilized for its FDA-approved purpose of treating obstructive sleep apnea as well as obesity.
This stipulation means that even though Zepbound is now acknowledged as a valid treatment under Medicare, patients may face hurdles. The prior authorization requirement—which necessitates insurers to approve drug use before it is dispensed—could become a point of contention. Hospitals and clinics will need to navigate this landscape carefully to ensure that treatments prescribed align with the accepted medical necessity standards.
Zepbound’s approval does not occur in isolation. This event resonates within a larger context in which pharmaceutical giants like Novo Nordisk have also made strides in producing effective weight loss medications. In fact, their product Wegovy, designed to promote weight loss while concurrently reducing cardiovascular risks, is permitted under similar coverage rules.
Moreover, both companies are exploring additional applications for their drugs—such as fatty liver disease and chronic kidney disease—though these ventures hinge on successful late-stage trial results and subsequent FDA approvals. Hence, while Zepbound’s approval for OSA marks a thrilling development, the evolving narrative of obesity treatments continues to gain momentum.
Medicaid coverage for Zepbound and comparable drugs presents a more complex picture. Coverage is contingent on the specific condition for which the drug is prescribed, alongside the stipulation that Eli Lilly must sign a Medicaid drug rebate agreement. This creates a variable landscape in which not all patients will have guaranteed access, particularly if the medication is prescribed solely for weight loss rather than for OSA.
It’s important to recognize how these dynamics play into broader healthcare affordability issues. The Biden administration’s recent proposal to allow Medicare and Medicaid to cover weight loss medications for obesity patients signals a possible shift towards more inclusive treatment options. However, the long-term ramifications—including a potential cost of $35 billion over a decade—raises questions about fiscal responsibility and the sustainability of such initiatives.
The approval of Zepbound by Medicare signifies excitement and opportunity in the treatment of obesity-linked obstructive sleep apnea. However, navigating the associated regulations presents complexities for health practitioners and patients alike. As policymakers grapple with the implications of expanding drug coverage in the realm of obesity treatment, the need for informed dialogue around healthcare access becomes increasingly vital. The discussion surrounding Zepbound serves as a reminder that while medical advancements herald change, the implications for real-world patient care require comprehensive and thoughtful approaches.

Leave a Reply