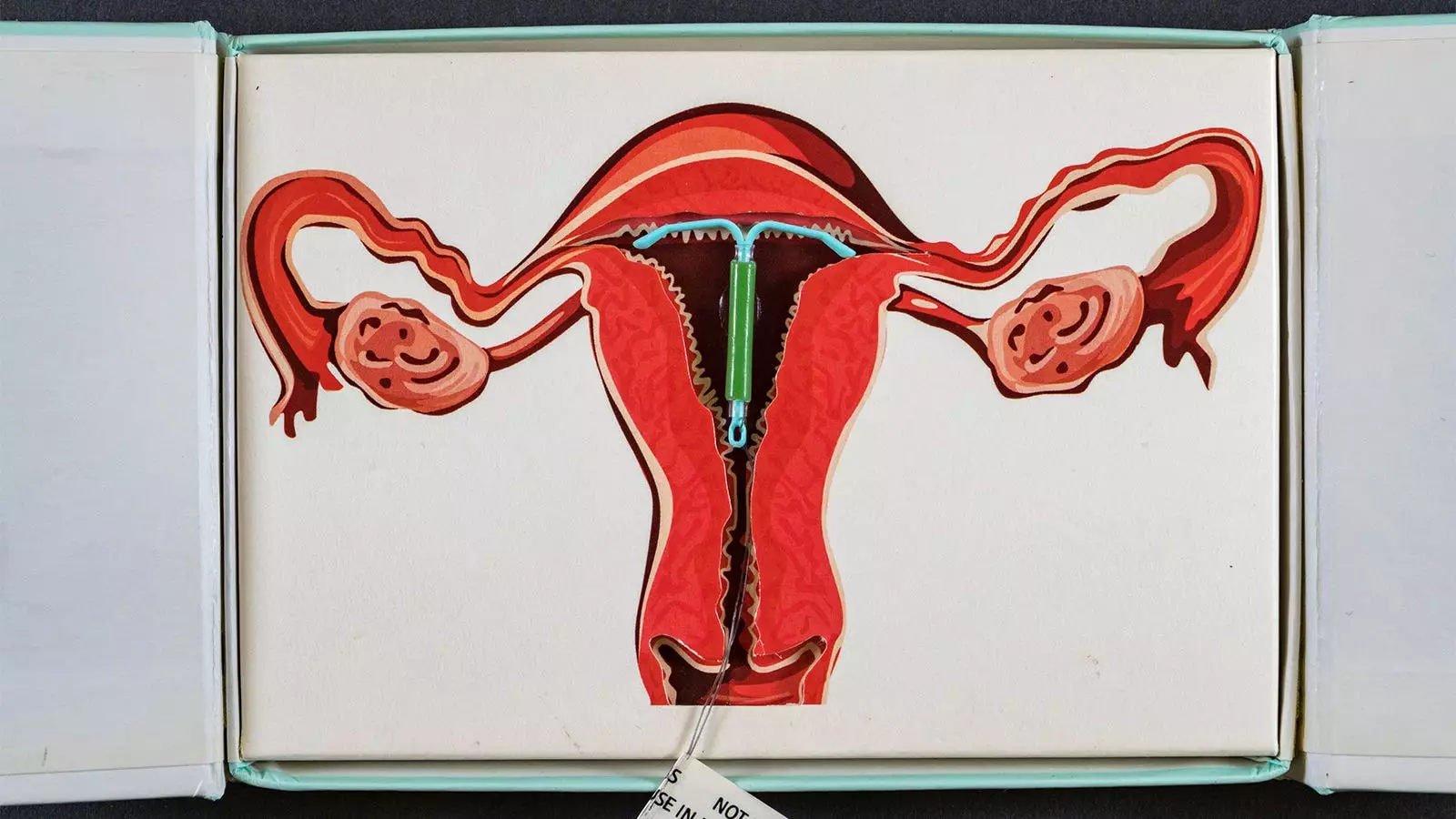
The ongoing discourse around contraceptive methods and their potential health implications remains a subject of close scrutiny and debate in the medical community. Recent research originating from Denmark provides a poignant examination of the relationship between levonorgestrel-releasing intrauterine devices (IUDs) and breast cancer risk in women under the age of 50. This investigation underscores a certain imperative: to critically assess not just the utility of hormonal contraceptives in reproductive health but also their long-term health repercussions, specifically concerning breast cancer.
The Danish study in question sought to determine the breast cancer risk associated with levonorgestrel-releasing IUDs, drawing upon an extensive dataset from national healthcare registries over a span of nearly two decades, from 2000 to 2019. The researchers focused on first-time users of these hormonal contraceptives, comprising 78,595 women who were matched with an equal number of non-users. A consistent comparative framework is vital for drawing meaningful conclusions, and this pairing of users and non-users provided a robust foundation for analyzing the implications of IUD usage.
It is essential to address that the study specifically targeted women aged 15-49, subsequently ruling out those who had used other forms of hormonal contraceptives within the previous five years. This careful selection mitigates the confounding effects that could arise from pre-existing hormonal exposures, ensuring a clearer insight into the direct relationship between the IUD and breast cancer risks.
Findings and Implications
Over the course of the study, involving almost 7 years of follow-up, the data unearthed critical insights: the use of levonorgestrel-releasing IUDs corresponded to a 40% elevated risk of developing breast cancer compared to non-users. Furthermore, this risk appeared to escalate with prolonged IUD usage. Women who utilized the device for a duration of 10 to 15 years faced an alarming 80% increase in breast cancer risk.
For clinicians and healthcare practitioners, these findings carry substantial weight as they highlight the necessity of informing patients about potential risks associated with long-term hormonal contraceptive use. There is a pervasive understanding among women of the benefits these contraceptives provide; however, the marginalization of their potential adverse effects can lead to uninformed decision-making. The authors of the study emphasize that the growing prevalence of levonorgestrel IUDs calls for comprehensive discussions about breast cancer risk alongside the benefits these devices offer.
The current study finds itself amid a broader tapestry of research regarding hormonal contraceptives and breast cancer. Other studies, including those examining hormonal contraceptives in BRCA1 gene carriers, have implicated similar risks, noting a significant relative risk increase among women who used any hormonal contraceptives. However, earlier studies lacked the granularity required to analyze risk stratification effectively based on the duration of usage.
The current analysis delineates breast cancer hazard ratios across various usage categories, affirming the nuanced relationship between the duration of IUD utilization and breast cancer diagnosis rates. Notably, while the report suggests particular hazards attached to longer use, the researchers also acknowledged limitations inherent in their findings; the lack of a dose-response relationship signals potential statistical imprecision or perhaps an absence of a causal link.
As this pivotal research sheds light on the interconnections between levonorgestrel-releasing IUD use and breast cancer risks, it unequivocally demands that healthcare providers engage in more thorough discussions with patients considering IUDs as a contraceptive option. Awareness of the potential health risks associated with prolonged use is paramount in enabling informed choices among women.
Future research endeavors will need to build upon this foundation. Investigating the multifactorial influences on breast cancer risk—including genetic factors, diet, and lifestyle—will yield a comprehensive understanding of how hormonal contraceptives interact within broader health contexts. Additionally, expanding this line of inquiry into diverse populations could help ascertain whether these findings are universally applicable or influenced by demographic variables.
In essence, as we advance our understanding of contraceptives and their implications, education and informed choice stand as the cornerstones of women’s health.

Leave a Reply