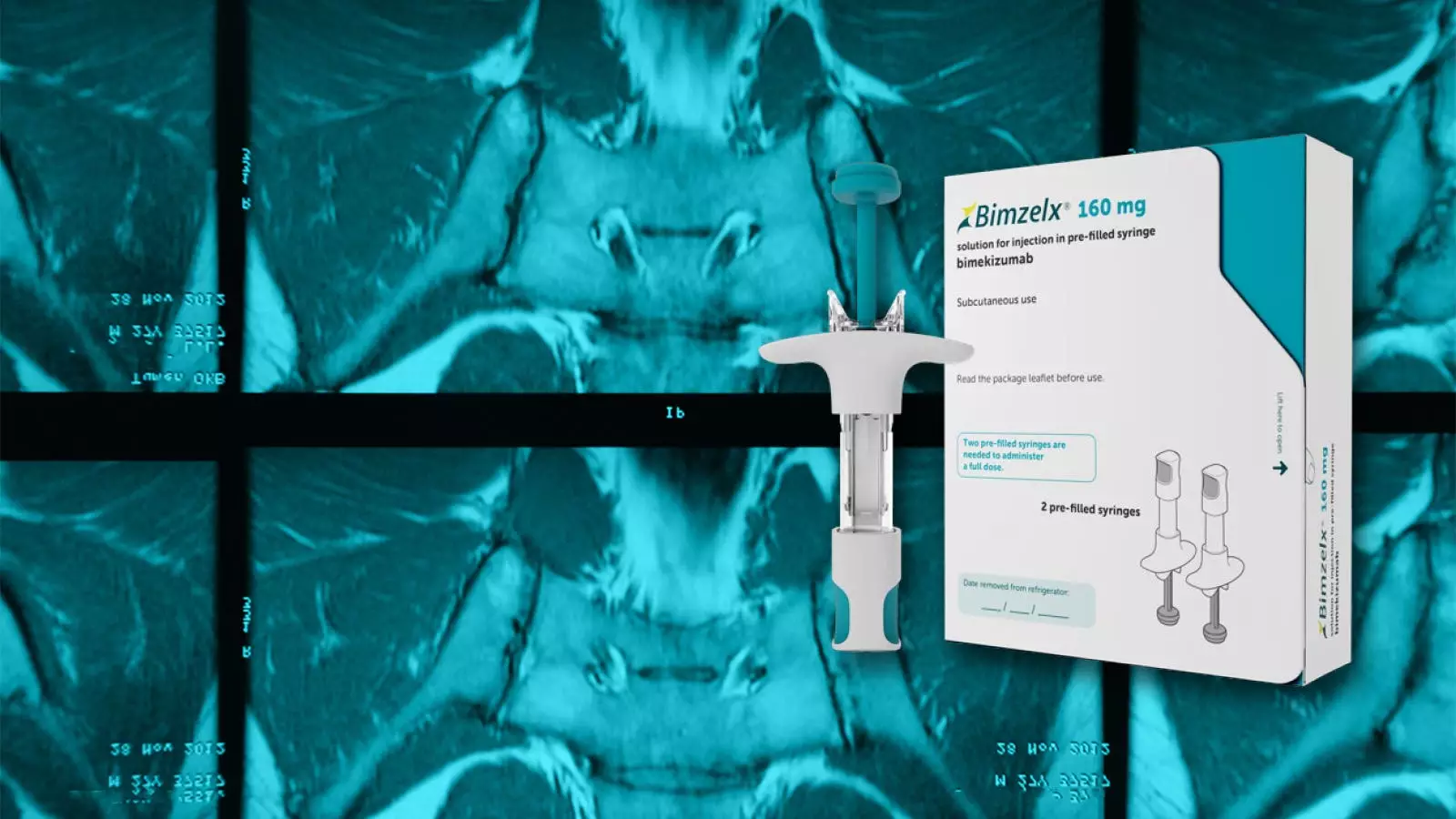
A recent study conducted by researchers has provided compelling evidence of the efficacy of bimekizumab, an interleukin-17 (IL-17) blocker, in the treatment of axial spondyloarthritis (axSpA). The trial, which spanned over 52 weeks, showcased strong efficacy of bimekizumab in improving the condition of patients with axSpA. More than 60% of patients demonstrated a 40% improvement in Assessment of SpondyloArthritis International Society ratings (ASAS40) after one year of continuous treatment. Interestingly, even patients who were initially randomized to placebo but later switched to the active drug achieved similar responses. These findings are published in Annals of the Rheumatic Diseases and are a significant development in the field of axSpA treatment.
Despite the promising results of bimekizumab, there are uncertainties about its availability in the U.S. market. While the drug has obtained marketing authorization for plaque psoriasis in many countries, it encountered manufacturing plant issues in Belgium, delaying its approval from the FDA. UCB Pharma, the developer of bimekizumab, anticipated resolving the problem; however, the timeline remains uncertain. It is crucial for UCB Pharma to overcome these obstacles to provide access to a potentially more effective treatment for axSpA patients.
One aspect that distinguishes bimekizumab from other biologics is its unique mechanism of action. Bimekizumab targets both IL-17A and IL-17F subspecies. While IL-17A is known for its high biological activity, IL-17F is enriched in the skin and synovial tissue of axSpA patients, making it an attractive secondary target for drug therapy. This differentiates bimekizumab from other IL-17A inhibitors, such as secukinumab, and raises hopes for increased effectiveness in treating axSpA.
The study, known as BE MOBILE 1 and BE MOBILE 2, included approximately 600 patients with clinical axSpA and radiographic axSpA, respectively. Participants were randomly assigned to receive either bimekizumab or placebo, without any background medications. The treatment lasted for 16 weeks, after which primary and secondary endpoints were evaluated. Patients who initially received placebo were then switched to the active drug, while the bimekizumab group continued their treatment. The mean patient age was around 40, with a majority being male. Notably, around 15% had previously used tumor necrosis factor inhibitors.
The primary efficacy endpoint of ASAS40 showed remarkable responses, with an improvement of at least 40% in more than 60% of patients after one year of continuous treatment with bimekizumab. The response rates continued to increase for certain subgroups throughout the 52 weeks, demonstrating the sustained efficacy of the drug. Other secondary measures, such as Ankylosing Spondylitis Disease Activity Score (ASDAS) and Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), also showed parallel improvements. Major improvements in ASDAS scores were observed in patients continuously on bimekizumab, while those who switched from placebo after 16 weeks also experienced significant improvements in their BASDAI scores.
In addition to assessing efficacy, the study also evaluated the safety profile of bimekizumab over the extended treatment period. While there was an increase in adverse events after the initial 16-week phase, discontinuations due to treatment-emergent adverse events (TEAEs) remained uncommon. The majority of events reported were relatively minor, such as nasopharyngitis and headache. However, infections, including fungal infections, were a concern, with 2% of participants experiencing serious infections, 8% developing oral candidiasis, and over 15% encountering fungal infections of any kind. Neutropenia was rare, affecting only approximately 1% of patients, and there were minimal occurrences of major cardiovascular events or malignancies. Overall, the safety data were consistent with previous evidence from clinical trials of bimekizumab in psoriasis and axSpA patients.
Bimekizumab has shown significant potential in improving the condition of patients with axSpA, as evident in the impressive results of the phase III trials. The drug’s ability to target both IL-17A and IL-17F subspecies could position it as a more effective treatment option compared to existing biologics. However, the delay in FDA approval for the U.S. market poses challenges for patients awaiting access to this innovative therapy. UCB Pharma must work diligently to resolve the manufacturing plant issues to ensure the timely availability of bimekizumab for patients in need.
Bimekizumab has demonstrated strong efficacy, with over 60% of patients experiencing significant improvement in axSpA symptoms after continuous treatment for one year. While uncertainties surrounding its availability in the U.S. market persist, the unique target of both IL-17A and IL-17F subspecies gives bimekizumab an edge over other biologics. The results of this study offer hope for improved outcomes in axSpA patients and highlight the importance of addressing manufacturing plant issues to expedite the approval process.

Leave a Reply